Amyloidosis is a rare disease that occurs when a substance called amyloid builds up in your organs. Amyloid is an abnormal protein that is usually produced in your bone marrow and can be deposited in any tissue or organ.
Amyloidosis can affect different organs in different people, and there are different types of amyloid. Amyloidosis frequently affects the heart, kidneys, liver, spleen, nervous system and digestive tract. Severe amyloidosis can lead to life-threatening organ failure.
Types of Amyloidosis:
The type of protein and where it collects determines the type of amyloidosis you have. Amyloid deposits may collect throughout your body or in just one area.
There are different types of amyloidosis, including:
Primary (systemic AL) amyloidosis. This occurs without a known cause, but it has been seen in people with a blood cancer called multiple myeloma. This is the most common type of amyloidosis.
Secondary (systemic AA) amyloidosis. This is the result of another chronic inflammatory disease, such as lupus, rheumatoid arthritis, tuberculosis, inflammatory bowel disease (Crohn's disease and ulcerative colitis), and certain cancers. It most commonly affects the spleen, kidneys, liver, adrenal gland, and lymph nodes.
Dialysis-related amyloidosis (DRA). This is more common in older adults and people who have been on dialysis for more than 5 years. This form of amyloidosis is caused by deposits of beta-2 microglobulin that build up in the blood.
Familial, or hereditary, amyloidosis (AF). This is a rare form that is passed down through families. It is caused by an abnormal amyloid transthyretin (TTR) protein, which is made in the liver. This protein is responsible for the most common forms of hereditary amyloidosis.
Senile systemic amyloidosis (SSA). This is caused deposits of normal TTR in the heart and other tissues. It occurs most commonly in older men.
Organ-specific amyloidosis. This is cause deposits of amyloid protein in single organs, including the skin (cutaneous amyloidosis).
Symptoms of Amyloidosis:
Changes in skin color
Clay-colored stools
Fatigue
Feeling of fullness
Joint pain
Low red blood cell count (anemia)
Shortness of breath
Swelling of the tongue
Tingling and numbness in legs and feet
Weak hand grip
Weakness
Weight loss
Treatment:
There's no cure for amyloidosis. However doctor will prescribe treatments to suppress the development of the amyloid-forming protein, and to manage your symptoms.
High-dose chemotherapy with stem cell transplant can help remove the substance that leads to amyloid formation in those with primary AL amyloidosis who have no more than two major organs damaged.
Secondary (AA) amyloidosis is treated by controlling the underlying disorder and with powerful anti-inflammatory medicines called steroids, which fight inflammation.
Liver transplant may stop the disease in those with hereditary amyloidosis.
A kidney or heart transplant may also be recommended.
Know About Common Disease, Know Use of Healthcare Analysis, Different Method Of health data Analysis
Friday, August 28, 2015
Thursday, August 27, 2015
Know About ‘Hepatitis’
CCS Category Name: Hepatitis
CCS Category Code: 6
ICD-9 Included (With Description):
ICD-9 Code ICD-9 Description
0700 HEPATITIS A WITH COMA
0701 HEPATITIS A W/O COMA
0702 HEPATITIS B WITH COMA (Begin 1980 End 1991)
07020 VRL HEPAT B CM W/O DELTA (Begin 1991)
07021 VRL HEPAT B CM W DELTA (Begin 1991)
07022 CHR HEPAT COMA W/O DELTA (Begin 1994)
CCS Category Code: 6
ICD-9 Included (With Description):
ICD-9 Code ICD-9 Description
0700 HEPATITIS A WITH COMA
0701 HEPATITIS A W/O COMA
0702 HEPATITIS B WITH COMA (Begin 1980 End 1991)
07020 VRL HEPAT B CM W/O DELTA (Begin 1991)
07021 VRL HEPAT B CM W DELTA (Begin 1991)
07022 CHR HEPAT COMA W/O DELTA (Begin 1994)
Know About ‘HIV infection’
‘HIV infection’ – commonly known “AIDs”.
HIV infection is a condition caused by the human immunodeficiency virus
(HIV). The condition gradually destroys the immune system, which makes
it harder for the body to fight infections.
How does HIV turn into AIDS?
Your immune system weakens as more CD4 cells are killed. You can have an HIV infection for years before it progresses to AIDS. People infected with HIV progress to AIDS when their CD4 count falls below 200 or they experience an AIDS-defining complication, such as: Pneumocystis pneumonia.
CCS Category Name: HIV infection
CCS Category Code: 5
ICD-9 Included (With Description):
ICD-9 Code ICD-9 Description
042 HIV DISEASE (Begin 1994)
0420 HIV W/SPECIF INFECTIONS (Begin 1986 End 1994)
0421 HIV CAUS OTH SPEC INFECT (Begin 1986 End 1994)
0422 HIV W/SPEC MALIG NEOPLSM (Begin 1986 End 1994)
0429 AIDS- UNSPECIFIED (Begin 1986 End 1994)
0430 HIV CAUS LYMPHADENOPATHY (Begin 1986 End 1994)
07953 HIV TYPE 2 (Begin 1993)
27910 IMMUNDEF T-CELL DEF NOS
27919 DEFIC CELL IMMUNITY NOS
79571 NONSPECIFIC SEROLOG HIV (Begin 1994)
7958 POSITIVE SERO/VIRAL HIV (Begin 1986 End 1994)
V08 HIV POSITIVE NOS (Begin 1994)
0431 HIV CAUS SP CNS DISEASE (Begin 1986 End 1994)
0432 HIV CAUS OT DISOR IMMUNE (Begin 1986 End 1994)
0433 HIV CAUS OTH SPECIF COND (Begin 1986 End 1994)
0439 ARC- UNSPECIFIED (Begin 1986 End 1994)
0440 HIV CAUS ACUTE INFECTION (Begin 1986 End 1994)
0449 HIV- UNSPECIFIED (Begin 1986 End 1994)
Disease Description:
Signs & Symptoms: Within a month or two of HIV entering the body, 40% to 90% of people experience flu like symptoms known as acute retroviral syndrome (ARS).
But sometimes HIV symptoms don't appear for years—sometimes even a decade—after infection.
Fever: One of the first signs of ARS can be a mild fever, up to about 102 degrees F. Fever accompanied by other usually mild symptoms, such as fatigue, swollen lymph glands, and a sore throat.
Fatigue: The inflammatory response generated by your besieged immune system also can cause you to feel tired and lethargic. Fatigue can be both an early and later sign of HIV.
Achy muscles, joint pain, swollen lymph nodes
Sore throat and headache
Skin Rash
Weight loss
Dry cough
Pneumonia
Night sweats
Nail changes
Yeast infections: Another fungal infection that's common in later stages is thrush, a mouth infection caused by Candida, a type of yeast.
Confusion or difficulty concentrating
Cold sores or genital herpes
Tingling and weakness
Menstrual irregularities
Stages Of HIV:
HIV infection comes in three stages.
The first stage is called acute infection or seroconversion, and it typically happens within two to six weeks after exposure or becoming infected. This is when the body's immune system puts up a fight against HIV.
After the first seroconversion period, the immune system loses the battle with HIV and symptoms go away. HIV infection goes into its second stage, which can be a long period without symptoms, called the asymptomatic (or latent ) period. This is when people may not know they are infected and can pass HIV on to others. This period can last 10 or more years.
AIDS (acquired immune deficiency syndrome) is the advanced stage of HIV infection. When the CD4 T-cell number drops below 200, people are diagnosed with AIDS.
Treatment Options: No cure exists, but medications can dramatically slow the disease's progress.
Antiviral drugs are used to prevent infections. E.g: Zidovudine (Retrovir), Emtricitabine/tenofovir, Lamivudine/zidovudine, Raltegravir, Efavirenz/emtricitabine/tenofovir (Atripla), Delavirdine, Abacavir/lamivudine/zidovudine (Trizivir), Efavirenz (Sustiva), Nevirapine (Viramune), Tenofovir (Viread), Maraviroc, Stavudine (Zerit), Lamivudine (Epivir), Abacavir (Ziagen), Etravirine (Intelence), Emtricitabine (Emtriva), Abacavir/lamivudine (Epzicom)
Other treatments: Enfuvirtide, Darunavir (Prezista), Amprenavir (Lexiva), Ritonavir (Norvir), Atazanavir (Reyataz)
How does HIV turn into AIDS?
Your immune system weakens as more CD4 cells are killed. You can have an HIV infection for years before it progresses to AIDS. People infected with HIV progress to AIDS when their CD4 count falls below 200 or they experience an AIDS-defining complication, such as: Pneumocystis pneumonia.
CCS Category Name: HIV infection
CCS Category Code: 5
ICD-9 Included (With Description):
ICD-9 Code ICD-9 Description
042 HIV DISEASE (Begin 1994)
0420 HIV W/SPECIF INFECTIONS (Begin 1986 End 1994)
0421 HIV CAUS OTH SPEC INFECT (Begin 1986 End 1994)
0422 HIV W/SPEC MALIG NEOPLSM (Begin 1986 End 1994)
0429 AIDS- UNSPECIFIED (Begin 1986 End 1994)
0430 HIV CAUS LYMPHADENOPATHY (Begin 1986 End 1994)
07953 HIV TYPE 2 (Begin 1993)
27910 IMMUNDEF T-CELL DEF NOS
27919 DEFIC CELL IMMUNITY NOS
79571 NONSPECIFIC SEROLOG HIV (Begin 1994)
7958 POSITIVE SERO/VIRAL HIV (Begin 1986 End 1994)
V08 HIV POSITIVE NOS (Begin 1994)
0431 HIV CAUS SP CNS DISEASE (Begin 1986 End 1994)
0432 HIV CAUS OT DISOR IMMUNE (Begin 1986 End 1994)
0433 HIV CAUS OTH SPECIF COND (Begin 1986 End 1994)
0439 ARC- UNSPECIFIED (Begin 1986 End 1994)
0440 HIV CAUS ACUTE INFECTION (Begin 1986 End 1994)
0449 HIV- UNSPECIFIED (Begin 1986 End 1994)
Disease Description:
Signs & Symptoms: Within a month or two of HIV entering the body, 40% to 90% of people experience flu like symptoms known as acute retroviral syndrome (ARS).
But sometimes HIV symptoms don't appear for years—sometimes even a decade—after infection.
Fever: One of the first signs of ARS can be a mild fever, up to about 102 degrees F. Fever accompanied by other usually mild symptoms, such as fatigue, swollen lymph glands, and a sore throat.
Fatigue: The inflammatory response generated by your besieged immune system also can cause you to feel tired and lethargic. Fatigue can be both an early and later sign of HIV.
Achy muscles, joint pain, swollen lymph nodes
Sore throat and headache
Skin Rash
Weight loss
Dry cough
Pneumonia
Night sweats
Nail changes
Yeast infections: Another fungal infection that's common in later stages is thrush, a mouth infection caused by Candida, a type of yeast.
Confusion or difficulty concentrating
Cold sores or genital herpes
Tingling and weakness
Menstrual irregularities
Stages Of HIV:
HIV infection comes in three stages.
The first stage is called acute infection or seroconversion, and it typically happens within two to six weeks after exposure or becoming infected. This is when the body's immune system puts up a fight against HIV.
After the first seroconversion period, the immune system loses the battle with HIV and symptoms go away. HIV infection goes into its second stage, which can be a long period without symptoms, called the asymptomatic (or latent ) period. This is when people may not know they are infected and can pass HIV on to others. This period can last 10 or more years.
AIDS (acquired immune deficiency syndrome) is the advanced stage of HIV infection. When the CD4 T-cell number drops below 200, people are diagnosed with AIDS.
Treatment Options: No cure exists, but medications can dramatically slow the disease's progress.
Antiviral drugs are used to prevent infections. E.g: Zidovudine (Retrovir), Emtricitabine/tenofovir, Lamivudine/zidovudine, Raltegravir, Efavirenz/emtricitabine/tenofovir (Atripla), Delavirdine, Abacavir/lamivudine/zidovudine (Trizivir), Efavirenz (Sustiva), Nevirapine (Viramune), Tenofovir (Viread), Maraviroc, Stavudine (Zerit), Lamivudine (Epivir), Abacavir (Ziagen), Etravirine (Intelence), Emtricitabine (Emtriva), Abacavir/lamivudine (Epzicom)
Other treatments: Enfuvirtide, Darunavir (Prezista), Amprenavir (Lexiva), Ritonavir (Norvir), Atazanavir (Reyataz)
Know About ‘Heart valve disorders’
CCS Category Name: Heart valve disorders
CCS Category Code: 96
ICD-9 Included (With Description):
ICD-9 Code ICD9-Descriotion
3940 MITRAL STENOSIS
3941 RHEUMATIC MITRAL INSUFF
3942 MITRAL STENOSIS W INSUFF
3949 MITRAL VALVE DIS NEC/NOS
3950 RHEUMAT AORTIC STENOSIS
3951 RHEUMATIC AORTIC INSUFF
7852 CARDIAC MURMURS NEC
7853 ABNORM HEART SOUNDS NEC
V422 HEART VALVE TRANSPLANT
V433 HEART VALVE REPLAC NEC
4241 AORTIC VALVE DISORDER
4242 NONRHEUM TRICUSP VAL DIS
4243 PULMONARY VALVE DISORDER
42490 ENDOCARDITIS NOS
42491 ENDOCARDITIS IN OTH DIS
42499 ENDOCARDITIS NEC
3968 MITR/AORTIC MULT INVOLV
3969 MITRAL/AORTIC V DIS NOS
3970 TRICUSPID VALVE DISEASE
3971 RHEUM PULMON VALVE DIS
3979 RHEUM ENDOCARDITIS NOS
4240 MITRAL VALVE DISORDER
3952 RHEUM AORTIC STEN/INSUFF
3959 RHEUM AORTIC DIS NEC/NOS
3960 MITRAL/AORTIC STENOSIS
3961 MITRAL STENOS/AORT INSUF
3962 MITRAL INSUF/AORT STENOS
3963 MITRAL/AORTIC VAL INSUFF
Disease Description: Heart valves regulate the flow of blood through the heart's four chambers—two small, round upper chambers (atria) and two larger, cone-shaped lower chambers (ventricles). Each ventricle has a inlet and a outlet valve. And both of these inlet and outlet valves are ‘one-way’. Each valve consists of flaps that open and close like one-way swinging doors.
These Heart valves can malfunction either by leaking or by or by not opening adequately and thus partially blocking the flow of blood through the valve. Either problem can greatly interfere with the heart's ability to pump blood.
What Are the Types of Valve Disease?
There are several types of valve disease:
Valvular stenosis. This occurs when a valve opening is smaller than normal due to stiff or fused leaflets. The narrowed opening may make the heart work very hard to pump blood through it. This can lead to heart failure and other symptoms (see below). All four valves can be stenotic (hardened, restricting blood flow); the conditions are called tricuspid stenosis, pulmonic stenosis, mitral stenosis or aortic stenosis.
Valvular insufficiency. Also called regurgitation, incompetence or "leaky valve", this occurs when a valve does not close tightly. If the valves do not seal, some blood will leak backwards across the valve. As the leak worsens, the heart has to work harder to make up for the leaky valve, and less blood may flow to the rest of the body. Depending on which valve is affected, the conditioned is called tricuspid regurgitation, pulmonary regurgitation, mitral regurgitation or aortic regurgitation.
Signs & Symptoms:
Shortness of breath and/or difficulty catching your breath.
Weakness or dizziness.
Discomfort in your chest.
Palpitations.
Swelling of your ankles, feet or abdomen.
Rapid weight gain.
Treatment Options:
Medical Treatment: Common Types of Medications used for 'Heart valve disorders' are: Diuretics, Antiarrhythmic medications, Vasodilators, ACE inhibitors, Beta blockers, Anticoagulants ("blood thinners")
Surgical Treatment: Depending upon results of different tests, the structure of your heart, your age, and your lifestyle will help your cardiologist (heart doctor), surgeon, and you decide what type of procedure will be best for you.
Surgical options include heart valve repair or replacement. Valves can be repaired or replaced with traditional heart valve surgery or a minimally invasive heart valve surgical procedure. Heart valves may also be repaired by other procedures such as percutaneous balloon valvotomy.
Procedure Suggested:
Procedure Code Procedure Description
3596 PERC HEART VALVULOPLASTY (Begin 1986)
3597 Perc mtrl vlv repr w imp (Begin 2010)
3599 OTHER HEART VALVE OPS
3500 CLOSED VALVOTOMY NOS
3501 CLOSED AORTIC VALVOTOMY
3502 CLOSED MITRAL VALVOTOMY
3503 CLOSED PULMON VALVOTOMY
3504 CLOSED TRICUSP VALVOTOMY
3505 Endovas repl aortc valve (Begin 2011)
3506 Trnsapcl rep aortc valve (Begin 2011)
3507 Endovas repl pulm valve (Begin 2011)
3508 Trnsapcl repl pulm valve (Begin 2011)
3509 Endovas repl uns hrt vlv (Begin 2011)
3510 OPEN VALVULOPLASTY NOS
3511 OPN AORTIC VALVULOPLASTY
3512 OPN MITRAL VALVULOPLASTY
3513 OPN PULMON VALVULOPLASTY
3514 OPN TRICUS VALVULOPLASTY
3520 REPLACE HEART VALVE NOS
3521 REPLACE AORT VALV-TISSUE
3522 REPLACE AORTIC VALVE NEC
3523 REPLACE MITR VALV-TISSUE
3524 REPLACE MITRAL VALVE NEC
3525 REPLACE PULM VALV-TISSUE
3526 REPLACE PULMON VALVE NEC
3527 REPLACE TRIC VALV-TISSUE
3528 REPLACE TRICUSP VALV NEC
CCS Category Code: 96
ICD-9 Included (With Description):
ICD-9 Code ICD9-Descriotion
3940 MITRAL STENOSIS
3941 RHEUMATIC MITRAL INSUFF
3942 MITRAL STENOSIS W INSUFF
3949 MITRAL VALVE DIS NEC/NOS
3950 RHEUMAT AORTIC STENOSIS
3951 RHEUMATIC AORTIC INSUFF
7852 CARDIAC MURMURS NEC
7853 ABNORM HEART SOUNDS NEC
V422 HEART VALVE TRANSPLANT
V433 HEART VALVE REPLAC NEC
4241 AORTIC VALVE DISORDER
4242 NONRHEUM TRICUSP VAL DIS
4243 PULMONARY VALVE DISORDER
42490 ENDOCARDITIS NOS
42491 ENDOCARDITIS IN OTH DIS
42499 ENDOCARDITIS NEC
3968 MITR/AORTIC MULT INVOLV
3969 MITRAL/AORTIC V DIS NOS
3970 TRICUSPID VALVE DISEASE
3971 RHEUM PULMON VALVE DIS
3979 RHEUM ENDOCARDITIS NOS
4240 MITRAL VALVE DISORDER
3952 RHEUM AORTIC STEN/INSUFF
3959 RHEUM AORTIC DIS NEC/NOS
3960 MITRAL/AORTIC STENOSIS
3961 MITRAL STENOS/AORT INSUF
3962 MITRAL INSUF/AORT STENOS
3963 MITRAL/AORTIC VAL INSUFF
Disease Description: Heart valves regulate the flow of blood through the heart's four chambers—two small, round upper chambers (atria) and two larger, cone-shaped lower chambers (ventricles). Each ventricle has a inlet and a outlet valve. And both of these inlet and outlet valves are ‘one-way’. Each valve consists of flaps that open and close like one-way swinging doors.
These Heart valves can malfunction either by leaking or by or by not opening adequately and thus partially blocking the flow of blood through the valve. Either problem can greatly interfere with the heart's ability to pump blood.
What Are the Types of Valve Disease?
There are several types of valve disease:
Valvular stenosis. This occurs when a valve opening is smaller than normal due to stiff or fused leaflets. The narrowed opening may make the heart work very hard to pump blood through it. This can lead to heart failure and other symptoms (see below). All four valves can be stenotic (hardened, restricting blood flow); the conditions are called tricuspid stenosis, pulmonic stenosis, mitral stenosis or aortic stenosis.
Valvular insufficiency. Also called regurgitation, incompetence or "leaky valve", this occurs when a valve does not close tightly. If the valves do not seal, some blood will leak backwards across the valve. As the leak worsens, the heart has to work harder to make up for the leaky valve, and less blood may flow to the rest of the body. Depending on which valve is affected, the conditioned is called tricuspid regurgitation, pulmonary regurgitation, mitral regurgitation or aortic regurgitation.
Signs & Symptoms:
Shortness of breath and/or difficulty catching your breath.
Weakness or dizziness.
Discomfort in your chest.
Palpitations.
Swelling of your ankles, feet or abdomen.
Rapid weight gain.
Treatment Options:
Medical Treatment: Common Types of Medications used for 'Heart valve disorders' are: Diuretics, Antiarrhythmic medications, Vasodilators, ACE inhibitors, Beta blockers, Anticoagulants ("blood thinners")
Surgical Treatment: Depending upon results of different tests, the structure of your heart, your age, and your lifestyle will help your cardiologist (heart doctor), surgeon, and you decide what type of procedure will be best for you.
Surgical options include heart valve repair or replacement. Valves can be repaired or replaced with traditional heart valve surgery or a minimally invasive heart valve surgical procedure. Heart valves may also be repaired by other procedures such as percutaneous balloon valvotomy.
Procedure Suggested:
Procedure Code Procedure Description
3596 PERC HEART VALVULOPLASTY (Begin 1986)
3597 Perc mtrl vlv repr w imp (Begin 2010)
3599 OTHER HEART VALVE OPS
3500 CLOSED VALVOTOMY NOS
3501 CLOSED AORTIC VALVOTOMY
3502 CLOSED MITRAL VALVOTOMY
3503 CLOSED PULMON VALVOTOMY
3504 CLOSED TRICUSP VALVOTOMY
3505 Endovas repl aortc valve (Begin 2011)
3506 Trnsapcl rep aortc valve (Begin 2011)
3507 Endovas repl pulm valve (Begin 2011)
3508 Trnsapcl repl pulm valve (Begin 2011)
3509 Endovas repl uns hrt vlv (Begin 2011)
3510 OPEN VALVULOPLASTY NOS
3511 OPN AORTIC VALVULOPLASTY
3512 OPN MITRAL VALVULOPLASTY
3513 OPN PULMON VALVULOPLASTY
3514 OPN TRICUS VALVULOPLASTY
3520 REPLACE HEART VALVE NOS
3521 REPLACE AORT VALV-TISSUE
3522 REPLACE AORTIC VALVE NEC
3523 REPLACE MITR VALV-TISSUE
3524 REPLACE MITRAL VALVE NEC
3525 REPLACE PULM VALV-TISSUE
3526 REPLACE PULMON VALVE NEC
3527 REPLACE TRIC VALV-TISSUE
3528 REPLACE TRICUSP VALV NEC
Tuesday, August 25, 2015
How the Single-level CCS Works
Single-level CCS is most useful
for ranking of diagnoses and procedures and for direct integration into
risk adjustment and other software. This Single-level CCS lassifies all
diagnoses and procedures into unique groups, has a total of 285 mutually
exclusive categories.
Now look for some Example of ‘Single-level CCS’
CCS Category CCS Category Desc
1 Tuberculosis
2 Septicemia (except in labor)
3 Bacterial infection; unspecified site
4 Mycoses
5 HIV infection
6 Hepatitis
7 Viral infection
8 Other infections; including parasitic
9 Sexually transmitted infections (not HIV or hepatitis)
10 Immunizations and screening for infectious disease
Now try to understand how the ICD-9 Rolled in each of the CCS Category:
CCS Category CCS Category Desc ICD9_diag_code ICD-9-CM CODE DESCRIPTION
5 HIV infection 0439 ARC- UNSPECIFIED (Begin 1986 End 1994)
5 HIV infection 0420 HIV W/SPECIF INFECTIONS (Begin 1986 End 1994)
5 HIV infection 0421 HIV CAUS OTH SPEC INFECT (Begin 1986 End 1994)
5 HIV infection 0422 HIV W/SPEC MALIG NEOPLSM (Begin 1986 End 1994)
5 HIV infection 0429 AIDS- UNSPECIFIED (Begin 1986 End 1994)
5 HIV infection 0430 HIV CAUS LYMPHADENOPATHY (Begin 1986 End 1994)
5 HIV infection 0431 HIV CAUS SP CNS DISEASE (Begin 1986 End 1994)
5 HIV infection 042 HIV DISEASE (Begin 1994)
5 HIV infection 0433 HIV CAUS OTH SPECIF COND (Begin 1986 End 1994)
5 HIV infection V08 HIV POSITIVE NOS (Begin 1994)
5 HIV infection 0440 HIV CAUS ACUTE INFECTION (Begin 1986 End 1994)
5 HIV infection 0449 HIV- UNSPECIFIED (Begin 1986 End 1994)
5 HIV infection 07953 HIV TYPE 2 (Begin 1993)
5 HIV infection 27910 IMMUNDEF T-CELL DEF NOS
5 HIV infection 27919 DEFIC CELL IMMUNITY NOS
5 HIV infection 79571 NONSPECIFIC SEROLOG HIV (Begin 1994)
5 HIV infection 7958 POSITIVE SERO/VIRAL HIV (Begin 1986 End 1994)
5 HIV infection 0432 HIV CAUS OT DISOR IMMUNE (Begin 1986 End 1994)
CCS Category CCS Category Desc ICD9_diag_code ICD-9-CM CODE DESCRIPTION
9 Sexually transmitted infections (not HIV or hepatitis) 0939 CARDIOVASCULAR SYPH NOS
9 Sexually transmitted infections (not HIV or hepatitis) 096 LATE SYPHILIS LATENT
9 Sexually transmitted infections (not HIV or hepatitis) 09482 SYPHILITIC PARKINSONISM
9 Sexually transmitted infections (not HIV or hepatitis) 09481 SYPHILITIC ENCEPHALITIS
9 Sexually transmitted infections (not HIV or hepatitis) 0943 ASYMPTOMAT NEUROSYPHILIS
9 Sexually transmitted infections (not HIV or hepatitis) 0942 SYPHILITIC MENINGITIS
9 Sexually transmitted infections (not HIV or hepatitis) 09484 SYPHILITIC OPTIC ATROPHY
9 Sexually transmitted infections (not HIV or hepatitis) 0940 TABES DORSALIS
9 Sexually transmitted infections (not HIV or hepatitis) 09485 SYPH RETROBULB NEURITIS
9 Sexually transmitted infections (not HIV or hepatitis) 09389 CARDIOVASCULAR SYPH NEC
9 Sexually transmitted infections (not HIV or hepatitis) 09382 SYPHILITIC MYOCARDITIS
9 Sexually transmitted infections (not HIV or hepatitis) 09381 SYPHILITIC PERICARDITIS
9 Sexually transmitted infections (not HIV or hepatitis) 09324 SYPHIL PULMONARY VALVE
9 Sexually transmitted infections (not HIV or hepatitis) 09323 SYPHIL TRICUSPID VALVE
The Other ICD-9 Codes that also used in CCS category 9 are:
09322,0941,0952,0900,0958,0957,0956,0955,09483,0953,0931,0951,0950,0949,09489,09487,09486, 0954,09049,0912,0911,0910,0909,0907,09321,0905,09150,09042,09041,09040,0903,0902,0901,0906, 0917,0970,0930,0929,0920,0919,09189,0913,09181,0914,09169,09162,09161,09152,09151,09320, 09182,09886,0959,0994,0993,0992,0991,09941,09889,09949,09885,09884,09883,09882,09881, 0987,0990,09956,79675,79519,79515,79505,0999,09940,09959,09853,09955,09954,09953,09952, 09951,09950,0998,09813,09830,0982,09819,09817,09816,0986,09814,09833,09812,09811,09810, 0980,0979,0971,09815,09840,79679,09852,09851,09850,09849,09843,09831,09841,09832,09839, 09837,09836,09835,09834,09859,09842
Now look for some Example of ‘Single-level CCS’
CCS Category CCS Category Desc
1 Tuberculosis
2 Septicemia (except in labor)
3 Bacterial infection; unspecified site
4 Mycoses
5 HIV infection
6 Hepatitis
7 Viral infection
8 Other infections; including parasitic
9 Sexually transmitted infections (not HIV or hepatitis)
10 Immunizations and screening for infectious disease
Now try to understand how the ICD-9 Rolled in each of the CCS Category:
CCS Category CCS Category Desc ICD9_diag_code ICD-9-CM CODE DESCRIPTION
5 HIV infection 0439 ARC- UNSPECIFIED (Begin 1986 End 1994)
5 HIV infection 0420 HIV W/SPECIF INFECTIONS (Begin 1986 End 1994)
5 HIV infection 0421 HIV CAUS OTH SPEC INFECT (Begin 1986 End 1994)
5 HIV infection 0422 HIV W/SPEC MALIG NEOPLSM (Begin 1986 End 1994)
5 HIV infection 0429 AIDS- UNSPECIFIED (Begin 1986 End 1994)
5 HIV infection 0430 HIV CAUS LYMPHADENOPATHY (Begin 1986 End 1994)
5 HIV infection 0431 HIV CAUS SP CNS DISEASE (Begin 1986 End 1994)
5 HIV infection 042 HIV DISEASE (Begin 1994)
5 HIV infection 0433 HIV CAUS OTH SPECIF COND (Begin 1986 End 1994)
5 HIV infection V08 HIV POSITIVE NOS (Begin 1994)
5 HIV infection 0440 HIV CAUS ACUTE INFECTION (Begin 1986 End 1994)
5 HIV infection 0449 HIV- UNSPECIFIED (Begin 1986 End 1994)
5 HIV infection 07953 HIV TYPE 2 (Begin 1993)
5 HIV infection 27910 IMMUNDEF T-CELL DEF NOS
5 HIV infection 27919 DEFIC CELL IMMUNITY NOS
5 HIV infection 79571 NONSPECIFIC SEROLOG HIV (Begin 1994)
5 HIV infection 7958 POSITIVE SERO/VIRAL HIV (Begin 1986 End 1994)
5 HIV infection 0432 HIV CAUS OT DISOR IMMUNE (Begin 1986 End 1994)
CCS Category CCS Category Desc ICD9_diag_code ICD-9-CM CODE DESCRIPTION
9 Sexually transmitted infections (not HIV or hepatitis) 0939 CARDIOVASCULAR SYPH NOS
9 Sexually transmitted infections (not HIV or hepatitis) 096 LATE SYPHILIS LATENT
9 Sexually transmitted infections (not HIV or hepatitis) 09482 SYPHILITIC PARKINSONISM
9 Sexually transmitted infections (not HIV or hepatitis) 09481 SYPHILITIC ENCEPHALITIS
9 Sexually transmitted infections (not HIV or hepatitis) 0943 ASYMPTOMAT NEUROSYPHILIS
9 Sexually transmitted infections (not HIV or hepatitis) 0942 SYPHILITIC MENINGITIS
9 Sexually transmitted infections (not HIV or hepatitis) 09484 SYPHILITIC OPTIC ATROPHY
9 Sexually transmitted infections (not HIV or hepatitis) 0940 TABES DORSALIS
9 Sexually transmitted infections (not HIV or hepatitis) 09485 SYPH RETROBULB NEURITIS
9 Sexually transmitted infections (not HIV or hepatitis) 09389 CARDIOVASCULAR SYPH NEC
9 Sexually transmitted infections (not HIV or hepatitis) 09382 SYPHILITIC MYOCARDITIS
9 Sexually transmitted infections (not HIV or hepatitis) 09381 SYPHILITIC PERICARDITIS
9 Sexually transmitted infections (not HIV or hepatitis) 09324 SYPHIL PULMONARY VALVE
9 Sexually transmitted infections (not HIV or hepatitis) 09323 SYPHIL TRICUSPID VALVE
The Other ICD-9 Codes that also used in CCS category 9 are:
09322,0941,0952,0900,0958,0957,0956,0955,09483,0953,0931,0951,0950,0949,09489,09487,09486, 0954,09049,0912,0911,0910,0909,0907,09321,0905,09150,09042,09041,09040,0903,0902,0901,0906, 0917,0970,0930,0929,0920,0919,09189,0913,09181,0914,09169,09162,09161,09152,09151,09320, 09182,09886,0959,0994,0993,0992,0991,09941,09889,09949,09885,09884,09883,09882,09881, 0987,0990,09956,79675,79519,79515,79505,0999,09940,09959,09853,09955,09954,09953,09952, 09951,09950,0998,09813,09830,0982,09819,09817,09816,0986,09814,09833,09812,09811,09810, 0980,0979,0971,09815,09840,79679,09852,09851,09850,09849,09843,09831,09841,09832,09839, 09837,09836,09835,09834,09859,09842
Know About CCS Or Clinical Classifications Software
 Clinical
Classifications Software (CCS) is another commonly used term in health
care sector. CCS collapses diagnosis and procedure codes from the ICD-9
Codes, which contains more than 14,000 diagnosis codes and 3,900
procedure codes.
Clinical
Classifications Software (CCS) is another commonly used term in health
care sector. CCS collapses diagnosis and procedure codes from the ICD-9
Codes, which contains more than 14,000 diagnosis codes and 3,900
procedure codes.This can be employed in many types of projects analyzing data on diagnoses and procedures. CCS can be used to identify populations for disease- or procedure-specific studies or to develop statistical reports providing information about relatively specific conditions.
Developed at the Agency for Healthcare Research and Quality (AHRQ), the Clinical Classifications Software (CCS) makes
CCS classification systems:
1. Single-level
2. Multi-level
Single-level : Single-level CCS is most useful for ranking of diagnoses and procedures and for direct integration into risk adjustment and other software. This Single-level CCS lassifies all diagnoses and procedures into unique groups, has a total of 285 mutually exclusive categories.
Multi-level: Multi-level CCS is most useful when evaluating larger aggregations of conditions and procedures or exploring them in greater detail. The multi-level CCS expands the single-level CCS into a hierarchical system. The multi-level CCS groups single-level CCS categories into broader body systems or condition categories. It also splits single-level CCS categories to provide more detail. The multi-level system has four levels for diagnoses and three levels for procedures, which provide the opportunity to examine general groupings or to assess very specific conditions and procedures.
Use of CCS:
CCS can be used with all clinical data that are coded using ICD-9-CM codes.
• Managed care plans utilize CCS to rank hospitalizations by type of condition. Managed care plan used CCS to examine numbers of cases, length of stay, and total costs, to better understand which conditions and procedures were associated with the highest resource use.
• Insurers use CCS to develop clinically-based utilization profiles.
• Researchers use CCS to explore the types of conditions and procedures that are most frequent in their study populations or to compare alternative treatments for similar conditions.
• Researchers also use CCS in risk adjustment models and as a way to predict future health resource utilization.
it easier to quickly understand patterns of diagnoses and procedures so that health plans, policy makers, and researchers can analyze costs, utilization, and outcomes associated with particular illnesses and procedures.
Monday, August 24, 2015
Know About Ambulatory-Care-Sensitive Admissions or PQI
Ambulatory-Care-Sensitive Admissions (ACSAs) are those that can be
prevented. This is also commonly known as Prevention Quality Indicators or in
short ‘PQI’.
The Agency for Healthcare Research and Quality (AHRQ) Quality Indicators (QIs) are
one Agency response to this need for a multidimensional, accessible family of quality indicators.
They include a family of measures that providers, policy makers, and researchers can use with
inpatient data to identify apparent variations in the quality of either inpatient or outpatient care.
The PQI composites provide:
-Provide assessment of quality and disparity
-Provide baselines to track progress
-Identify information gaps
-Emphasize interdependence of quality and disparities
-Promote awareness and change
What AHRQ PQI Composite Measure:
PQI #01 Diabetes Short-Term Complications Admission Rate
PQI #03 Diabetes Long-Term Complications Admission Rate
PQI #05 Chronic Obstructive Pulmonary Disease (COPD) or Asthma in Older Adults Admission Rate
PQI #07 Hypertension Admission Rate
PQI #08 Congestive Heart Failure (CHF) Admission Rate
PQI #10 Dehydration Admission Rate
PQI #11 Bacterial Pneumonia Admission Rate
PQI #12 Urinary Tract Infection Admission Rate
PQI #13 Angina without Procedure Admission Rate
PQI #14 Uncontrolled Diabetes Admission Rate
PQI #15 Asthma in Younger Adults Admission Rate
PQI #16 Rate of Lower-Extremity Amputation Among Patients With Diabetes
Acute Composite (PQI #91)
PQI #10 Dehydration Admission Rate
PQI #11 Bacterial Pneumonia Admission Rate
PQI #12 Urinary Tract Infection Admission Rate
Chronic Composite (PQI #92)
PQI #01 Diabetes Short-Term Complications Admission Rate
PQI #03 Diabetes Long-Term Complications Admission Rate
PQI #05 Chronic Obstructive Pulmonary Disease (COPD) or Asthma in Older Adults Admission Rate
PQI #07 Hypertension Admission Rate
PQI #08 Congestive Heart Failure (CHF) Admission Rate
PQI #13 Angina without Procedure Admission Rate
PQI #14 Uncontrolled Diabetes Admission Rate
PQI #15 Asthma in Younger Adults Admission Rate
PQI #16 Rate of Lower-Extremity Amputation Among Patients With Diabetes
The Agency for Healthcare Research and Quality (AHRQ) Quality Indicators (QIs) are
one Agency response to this need for a multidimensional, accessible family of quality indicators.
They include a family of measures that providers, policy makers, and researchers can use with
inpatient data to identify apparent variations in the quality of either inpatient or outpatient care.
The PQI composites provide:
-Provide assessment of quality and disparity
-Provide baselines to track progress
-Identify information gaps
-Emphasize interdependence of quality and disparities
-Promote awareness and change
What AHRQ PQI Composite Measure:
PQI #01 Diabetes Short-Term Complications Admission Rate
PQI #03 Diabetes Long-Term Complications Admission Rate
PQI #05 Chronic Obstructive Pulmonary Disease (COPD) or Asthma in Older Adults Admission Rate
PQI #07 Hypertension Admission Rate
PQI #08 Congestive Heart Failure (CHF) Admission Rate
PQI #10 Dehydration Admission Rate
PQI #11 Bacterial Pneumonia Admission Rate
PQI #12 Urinary Tract Infection Admission Rate
PQI #13 Angina without Procedure Admission Rate
PQI #14 Uncontrolled Diabetes Admission Rate
PQI #15 Asthma in Younger Adults Admission Rate
PQI #16 Rate of Lower-Extremity Amputation Among Patients With Diabetes
Acute Composite (PQI #91)
PQI #10 Dehydration Admission Rate
PQI #11 Bacterial Pneumonia Admission Rate
PQI #12 Urinary Tract Infection Admission Rate
Chronic Composite (PQI #92)
PQI #01 Diabetes Short-Term Complications Admission Rate
PQI #03 Diabetes Long-Term Complications Admission Rate
PQI #05 Chronic Obstructive Pulmonary Disease (COPD) or Asthma in Older Adults Admission Rate
PQI #07 Hypertension Admission Rate
PQI #08 Congestive Heart Failure (CHF) Admission Rate
PQI #13 Angina without Procedure Admission Rate
PQI #14 Uncontrolled Diabetes Admission Rate
PQI #15 Asthma in Younger Adults Admission Rate
PQI #16 Rate of Lower-Extremity Amputation Among Patients With Diabetes
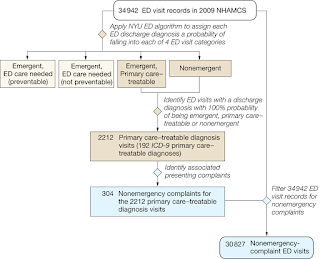
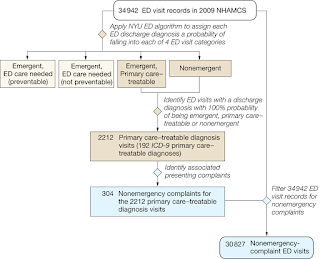
How to Read the NYU-ED algorithm Output file
All three versions of the ED algorithm programming – the Access, SAS, and SPSS versions – will produce a microdata (record-level) file, with one record for each encounter record in your ED database.)
The output microdata file will simply have a new set of variables in addition to your original data set variables. The names of the new variables are:
• ne = “Non-emergent”
• epct = “Emergent/Primary Care Treatable”
• edcnpa = “Emergent ED Care Needed Preventable/Avoidable”
• edcnnpa = “Emergent ED Care Needed Not Preventable/Avoidable”
• injury = “Injury principal diagnoses”
• psych = “Mental health principal diagnoses”
• alcohol = “Alcohol-related health principal diagnoses”
• drug = “Drug-related health principal diagnoses (excluding alcohol)”
• unclassified = “Not classified - not in one of the above categories”
View -
For example, in the case of urinary tract infections (ICD-9-CM code 599.0), each case is assigned 66% “non-emergent”, 17% “emergent/primary care treatable”, and 17% “emergent - ED care needed - preventable/avoidable”. The sum of the values in the new data fields will always total 1, and the injury, psych, alcohol, drug, and unclassified fields are always binary (equal to 1 or 0).
The output microdata file will simply have a new set of variables in addition to your original data set variables. The names of the new variables are:
• ne = “Non-emergent”
• epct = “Emergent/Primary Care Treatable”
• edcnpa = “Emergent ED Care Needed Preventable/Avoidable”
• edcnnpa = “Emergent ED Care Needed Not Preventable/Avoidable”
• injury = “Injury principal diagnoses”
• psych = “Mental health principal diagnoses”
• alcohol = “Alcohol-related health principal diagnoses”
• drug = “Drug-related health principal diagnoses (excluding alcohol)”
• unclassified = “Not classified - not in one of the above categories”
View -
New York University Emergency Department visit severity algorithm
For each ED encounter, the numbers in the new fields represent the relative percentage of cases for that diagnosis falling into the various classification categories.For example, in the case of urinary tract infections (ICD-9-CM code 599.0), each case is assigned 66% “non-emergent”, 17% “emergent/primary care treatable”, and 17% “emergent - ED care needed - preventable/avoidable”. The sum of the values in the new data fields will always total 1, and the injury, psych, alcohol, drug, and unclassified fields are always binary (equal to 1 or 0).
Wednesday, August 19, 2015
Surgon Left Medical Items In woman's Stomach During Operation
Relatives of a patient in Pakistan claims surgeons left medical Items in her relative's body after a stomach operation. The patient was suffering from severe pain after the operation. The relatives then came to the hospital outdoor and beat up the hospital staff. They also vandalized the office.
HOW YOU CAN APPLY ED Algorithm
There are couple of different analytical platform that you can use to apply ED/ER Algorithm. The most commons are Microsoft Access 2000 Version and SAS or SPSS Version.
 USE Microsoft Access 2000 Version:
USE Microsoft Access 2000 Version:
The Microsoft Access version of the ED algorithm contained a total of 2 files - “NYU ED Algorithm X.X.MDB" and NYUED.HLP.
Users need to place the two files in the same directory of the computer, open the file using Microsoft Access. All further instructions can then be accessed by pressing F1 on your keyboard. Context-specific help can be accessed after selected each menu choice, EXCEPT for the "Import a Dataset" menu choice. To access help for that function, user need to use F1 button when viewing the main menu, and then select "Import a Dataset" from Help Table of Contents.
This version of the ED algorithm requires that your ED dataset be available in ASCII (text), Access, .DBF, or Excel format.
Using the SAS or SPSS Version:
For the SPSS version, the files are:
• “DX GROUPS.SAV” - This file is merged onto your ED data in order to recode and group diagnoses;
• ‘EDDXS.SAV" - This file lists diagnoses and the proportion of cases that are to be assigned to the classification categories; and
• “ED Algorithm.sps” - This is the SPSS program that is used to run the algorithm.
For the SAS version (which will run in either SAS 7 or SAS 8), the files are:
• “ED Macros.sas” - This file contains SAS macros that group or recode diagnoses and classify them into the categories described above;
• ‘FINDXACS.SD7" - This file lists diagnoses and the proportion of cases that are to be assigned to the classification categories; and
• “ED Algorithm Sample Program.sas” - This is the SAS program that is used to run the algorithm.
All files are contained in the compressed (zipped) file.
Applying the algorithm involves three simple steps:
STEP 1: Put the unzipped files in a directory along with the ED encounter data set you want to classify (containing one record for each ED visit). The ED data set should be in the appropriate format (SAS 7 or 8, or SPSS) and contain a variable with the principal discharge diagnosis for the ED visit.
STEP 2: Set the appropriate names in the LET statements at the top of the program.
For the SPSS version, specify the following: 1) IN SINGLE QUOTES, the full path name (including a final backslash) of the directory on your computer that contains the files, 2) IN SINGLE QUOTES, the name of the SPSS data set (including the .SAV extension) containing ED records to be classified, 3) the name of the variable in your data set that contains the principal diagnosis, and 4) IN SINGLE QUOTES, the name you want the program to use to write the output data set (including the .SAV extension).
STEP 3: Run the program and analyze the output data set, which will be written to the same directory the other files are in.
 USE Microsoft Access 2000 Version:
USE Microsoft Access 2000 Version:The Microsoft Access version of the ED algorithm contained a total of 2 files - “NYU ED Algorithm X.X.MDB" and NYUED.HLP.
Users need to place the two files in the same directory of the computer, open the file using Microsoft Access. All further instructions can then be accessed by pressing F1 on your keyboard. Context-specific help can be accessed after selected each menu choice, EXCEPT for the "Import a Dataset" menu choice. To access help for that function, user need to use F1 button when viewing the main menu, and then select "Import a Dataset" from Help Table of Contents.
This version of the ED algorithm requires that your ED dataset be available in ASCII (text), Access, .DBF, or Excel format.
Using the SAS or SPSS Version:
For the SPSS version, the files are:
• “DX GROUPS.SAV” - This file is merged onto your ED data in order to recode and group diagnoses;
• ‘EDDXS.SAV" - This file lists diagnoses and the proportion of cases that are to be assigned to the classification categories; and
• “ED Algorithm.sps” - This is the SPSS program that is used to run the algorithm.
For the SAS version (which will run in either SAS 7 or SAS 8), the files are:
• “ED Macros.sas” - This file contains SAS macros that group or recode diagnoses and classify them into the categories described above;
• ‘FINDXACS.SD7" - This file lists diagnoses and the proportion of cases that are to be assigned to the classification categories; and
• “ED Algorithm Sample Program.sas” - This is the SAS program that is used to run the algorithm.
All files are contained in the compressed (zipped) file.
Applying the algorithm involves three simple steps:
STEP 1: Put the unzipped files in a directory along with the ED encounter data set you want to classify (containing one record for each ED visit). The ED data set should be in the appropriate format (SAS 7 or 8, or SPSS) and contain a variable with the principal discharge diagnosis for the ED visit.
STEP 2: Set the appropriate names in the LET statements at the top of the program.
For the SPSS version, specify the following: 1) IN SINGLE QUOTES, the full path name (including a final backslash) of the directory on your computer that contains the files, 2) IN SINGLE QUOTES, the name of the SPSS data set (including the .SAV extension) containing ED records to be classified, 3) the name of the variable in your data set that contains the principal diagnosis, and 4) IN SINGLE QUOTES, the name you want the program to use to write the output data set (including the .SAV extension).
STEP 3: Run the program and analyze the output data set, which will be written to the same directory the other files are in.
Sunday, August 16, 2015
Know About NYU classification
NYU classification or commonly used as ED Classification is the way to classify Emergency utilization. With support from the Commonwealth Fund, the Robert Wood Johnson Foundation, and the United Hospital Fund of New York, the NYU Center for Health and Public Service Research has developed an algorithm to help classify ED utilization.
ED Or NYU categories:
• Non-emergent - The patient’s initial complaint, presenting symptoms, vital signs, medical history, and age indicated that immediate medical care was not required within 12 hours;
• Emergent/Primary Care Treatable - Based on information in the record, treatment was required within 12 hours, but care could have been provided effectively and safely in a primary care setting. The complaint did not require continuous observation, and no procedures were performed or resources used that are not available in a primary care setting (e.g., CAT scan or certain lab tests);
• Emergent - ED Care Needed - Preventable/Avoidable - Emergency department care was required based on the complaint or procedures performed/resources used, but the emergent nature of the condition was potentially preventable/avoidable if timely and effective ambulatory care had been received during the episode of illness (e.g., the flare-ups of asthma, diabetes, congestive heart failure, etc.); and
• Emergent - ED Care Needed - Not Preventable/Avoidable - Emergency department care was required and ambulatory care treatment could not have prevented the condition (e.g., trauma, appendicitis, myocardial infarction, etc.).
It is important to recognize that the algorithm is not intended as a triage tool or a mechanism to determine whether ED use in a specific case is “appropriate” (e.g., for reimbursement purposes). Since few diagnostic categories are clear-cut in all cases, the algorithm assigns cases probabilistically on a percentage basis, reflecting this potential uncertainty and variation.
Since the original development of the algorithm, users have expressed an interest in examining separately cases involving a primary diagnosis of injury, mental health problems, alcohol, or substance abuse.
ED Or NYU categories:
• Non-emergent - The patient’s initial complaint, presenting symptoms, vital signs, medical history, and age indicated that immediate medical care was not required within 12 hours;
• Emergent/Primary Care Treatable - Based on information in the record, treatment was required within 12 hours, but care could have been provided effectively and safely in a primary care setting. The complaint did not require continuous observation, and no procedures were performed or resources used that are not available in a primary care setting (e.g., CAT scan or certain lab tests);
• Emergent - ED Care Needed - Preventable/Avoidable - Emergency department care was required based on the complaint or procedures performed/resources used, but the emergent nature of the condition was potentially preventable/avoidable if timely and effective ambulatory care had been received during the episode of illness (e.g., the flare-ups of asthma, diabetes, congestive heart failure, etc.); and
• Emergent - ED Care Needed - Not Preventable/Avoidable - Emergency department care was required and ambulatory care treatment could not have prevented the condition (e.g., trauma, appendicitis, myocardial infarction, etc.).
It is important to recognize that the algorithm is not intended as a triage tool or a mechanism to determine whether ED use in a specific case is “appropriate” (e.g., for reimbursement purposes). Since few diagnostic categories are clear-cut in all cases, the algorithm assigns cases probabilistically on a percentage basis, reflecting this potential uncertainty and variation.
Since the original development of the algorithm, users have expressed an interest in examining separately cases involving a primary diagnosis of injury, mental health problems, alcohol, or substance abuse.
Thursday, August 13, 2015
What IS CCS Classification!!
Clinical Classifications Software (CCS) is a tool for clustering patient diagnoses and procedures into a manageable number of clinically meaningful categories. This was developed by Agency for Healthcare Research and Quality (AHRQ).
CCS is used to analyze costs, usage, and outcomes associated with patient diagnoses and procedures.
CCS is composed of diagnoses and procedures categories, which are organized in two related classification systems. The single-level system consists of 285 mutually-exclusive diagnosis categories, 231 mutually-exclusive procedure categories, and no hierarchical structure. The multi-level system uses the single-level categories and International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes in a hierarchical system consisting of four levels for diagnoses and three levels for procedures. This "clinical grouper" makes it easier to quickly understand patterns of diagnoses and procedures so that health plans, policy makers, and researchers can analyze costs, utilization, and outcomes associated with particular illnesses and procedures.
How Often id Updates?
CCS is updated annually.
How Is CCS Used?
Clinical Classifications Software can be used with all clinical data that are coded using ICD-9-CM codes. CCS is used in a variety of ways:
Managed care plans utilize CCS to rank hospitalizations by type of condition. One managed care plan used CCS to examine numbers of cases, length of stay, and total costs, to better understand which conditions and procedures were associated with the highest resource use.
Insurers use CCS to develop clinically-based utilization profiles. For example, one insurer integrated CCS into in-house software that develops profiles of patient populations and purchasers.
Researchers use CCS to explore the types of conditions and procedures that are most frequent in their study populations or to compare alternative treatments for similar conditions. In one study of differences in use of procedures among payers, CCS procedure categories provided a convenient grouping scheme.
Researchers also use CCS in risk adjustment models and as a way to predict future health resource utilization. Investigators in one study found that categorizing patients using CCS predicted more than 40 percent of the subsequent year's medical expenses.
CCS is used to analyze costs, usage, and outcomes associated with patient diagnoses and procedures.
CCS is composed of diagnoses and procedures categories, which are organized in two related classification systems. The single-level system consists of 285 mutually-exclusive diagnosis categories, 231 mutually-exclusive procedure categories, and no hierarchical structure. The multi-level system uses the single-level categories and International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes in a hierarchical system consisting of four levels for diagnoses and three levels for procedures. This "clinical grouper" makes it easier to quickly understand patterns of diagnoses and procedures so that health plans, policy makers, and researchers can analyze costs, utilization, and outcomes associated with particular illnesses and procedures.
How Often id Updates?
CCS is updated annually.
How Is CCS Used?
Clinical Classifications Software can be used with all clinical data that are coded using ICD-9-CM codes. CCS is used in a variety of ways:
Managed care plans utilize CCS to rank hospitalizations by type of condition. One managed care plan used CCS to examine numbers of cases, length of stay, and total costs, to better understand which conditions and procedures were associated with the highest resource use.
Insurers use CCS to develop clinically-based utilization profiles. For example, one insurer integrated CCS into in-house software that develops profiles of patient populations and purchasers.
Researchers use CCS to explore the types of conditions and procedures that are most frequent in their study populations or to compare alternative treatments for similar conditions. In one study of differences in use of procedures among payers, CCS procedure categories provided a convenient grouping scheme.
Researchers also use CCS in risk adjustment models and as a way to predict future health resource utilization. Investigators in one study found that categorizing patients using CCS predicted more than 40 percent of the subsequent year's medical expenses.
Subscribe to:
Posts (Atom)






